
300 mg/2 ml, 600 mg/4 ml
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
DACLIN (Clindamycin phosphate) is a semi-synthetic antibiotic produced by a 7(S)-chloro- substitution of the 7(R)-hydroxyl group of the parent compound lincomycin. Chemically, Clindamycin phosphate is Methyl 7-chloro-6,7,8-trideoxy-6-(1-methyl-trans-4-propyl- L-2 pyrrolidinecarboxamido)-1-thio- L-threo- - D -galacto-octopyranoside 2-(dihydrogen phosphate). Its molecular formula is C18H34ClN2O8PS and molecular weight is 504.97.
STRUCTURAL FORMULA :
Its structural formula is :
-Structure.jpg)
DACLIN is a clear, colourless to pale yellow solution filled in flint ampoule of suitable size.
COMPOSITION :
Each ml contains :
Clindamycin Phosphate (anhydrous) USP
equivalent to Clindamycin 150 mg
Benzyl Alcohol I.P. 0.9 % v/v
(as preservative)
Water for Injection I.P q.s.
ACTIONS :
Clindamycin is a lincosamide antibiotic with a primarily bacteriostatic action against gram-positive aerobes and a wide range of anaerobic bacteria. Lincosamides such as Clindamycin bind to the 50S subunit of the bacterial ribosome similarly to macrolides such as erythromycin and inhibit the early stages of protein synthesis. The action of Clindamycin is predominantly bacteriostatic although high concentrations may be slowly bactericidal against sensitive strains. Most gram-negative aerobic bacteria, including the Enterobacteriaceae, are resistant to Clindamycin. Clindamycin demonstrates cross-resistance with lincomycin. When tested by in vitro methods, some staphylococcal strains originally resistant to erythromycin rapidly developed resistance to Clindamycin. The mechanisms for resistance are the same as for erythromycin, namely methylation of the ribosomal binding site, chromosomal mutation of the ribosomal protein and in a few staphylococcal isolates enzymic inactivation by a plasmid-mediated adenyltransferase.
PHARMACOKINETICS :
On parenteral administration, the phosphate ester is rapidly hydrolyzed to the active parent compound. Following intramuscular injection, peak plasma concentrations are only attained after 3 hours in adults and 1 hour in children. The peak plasma concentrations obtained following intramuscular administration are : 6 µg/mL with a 300 mg dose and 9 µg/mL with a 600 mg dose in adults. Immediately after a 20 - 45 minute intravenous infusion of 600 mg, the plasma concentrations is approximately 10 µg/mL. The half-life of Clindamycin is about 2,7 hours and modest accumulation is thus expected to occur if it is given every 6 hours. The half-life may be lengthened in patients with impaired renal function, and dosage in these patients should be adjusted according to plasma concentrations. Accumulation may also occur in patients with hepatic failure. Clindamycin is 90 % plasma protein bound. It is widely distributed in many fluids and tissues including bone, but not in sufficient concentrations in the cerebrospinal fluid. It does however cross the placental barrier. It accumulates in polymorphonuclear leukocytes and alveolar macrophages and is also concentrated in abscesses in experimental animals. About 10 % of Clindamycin is excreted unaltered in the urine and small quantities are to be found in the faeces.
INDICATIONS :
Clindamycin phosphate has been shown to be effective in the treatment of the following infections when caused by susceptible anaerobic bacteria or susceptible strains of gram-positive bacteria such as streptococci, staphylococci and pneumococci :
1. Upper respiratory infections including tonsillitis, pharyngitis, sinusitis, otitis media and scarlet fever.
2. Lower respiratory infections including bronchitis, pneumonia, emphyema and lung abscess.
3. Skin and soft tissue infections including acne, furuncles, cellulitis, impetigo, abscesses, and wound infections. For specific skin and soft tissue infections like erysipelas and paronychia (panaritium), it would seem logical that these conditions would respond very well to Clindamycin therapy.
4. Bone and joint infections including osteomyelitis and septic arthritis.
5. Pelvic infections including endometritis, cellulitis, vaginal cuff infection tubo-ovarian abscesses salpingitis and pelvic inflammatory disease when given in conjunction with an antibiotic of appropriate gram negative aerobic spectrum. In cases of cervicitis due to Chlamydia trachomatis, mono therapy with clindamycin has been shown to be effective in eradicating the organism.
6. Intra-abdominal infections including peritonitis and abdominal abscess when given in conjunction with an antibiotic of appropriate gram-negative aerobic spectrum.
7. Septicemia and endocarditis - the effectiveness of Clindamycin in the treatment of selected cases of endocarditis has been documented when Clindamycin is determined to be bactericidal to the infecting organism by in vitro testing of appropriate achievable serum concentrations.
8. Dental infections such as periodental abscess and periodonitis.
9. Toxoplasmic encephalitis in patients with AIDS. In patients who are intolerant to conventional treatment, Clindamycin in combination with pyrimethamine has been shown to be efficacious.
10. Pneumocystis carinii pneumonia in patients with AIDS. In patients who are intolerant to or do not respond to conventional treatment, Clindamycin in combination with primaquine has been shown to be efficacious.
Administration :
I.M. or I.V. administration (If given intravenously must be diluted before use).
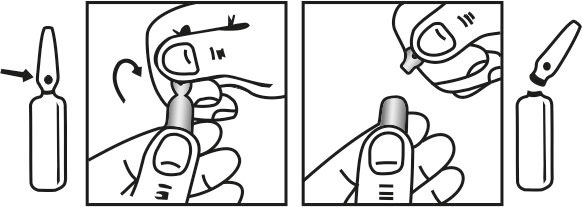
INSTRUCTION FOR USE OF AMPOULE :
The ampoule used in this product is equipped with O.P.C (One Point Cut) opening system. No ampoule file is needed to open the ampoule. The neck of the ampoule is prescored at the point of constriction. A coloured dot on the ampoule head helps to orient the ampoule. Take the ampoule and face the coloured dot. Let the solution at the head of the ampoule to flow down by shaking or a gentle stroke. The ampoule opens easily by placing the thumb on the coloured dot and gently pressing downwards as shown.
Dosage :
Adults :
Parenteral (I.M. or I.V. administration)
Mild infections or infections due to highly susceptible pathogens : 600 mg/day in 2 equal doses. Moderately severe infections : 600-1200 mg/day in 2, 3 or 4 equal doses. Severe infections : 1200-2700 mg/day in 2, 3 or 4 equal doses.
Note : For more serious infections, these doses may have to be increased. In life-threatening situations, doses of as much as 4,8 grams daily have been given intravenously to adults. See “Dilution and Infusion Rates” section below. Alternatively, drug may be administered in the form of a single rapid infusion of the first dose followed by continuous I.V. infusion as follows :
-Table.jpg)
COMPATIBILITY / INCOMPATIBILITY :
DACLIN has been known to be physically and chemically compatible for at least 24 hours in glucose 5 % water and sodium chloride injection solutions containing the following antibiotics in usually administered concentrations :
Amikacin sulfate, aztreonam, cephamandole nafate, cefazolin sodium, cefotaxime sodium, cefoxitin sodium, ceftazidime sodium, ceftizoxime sodium, gentamicin sulfate, netilmicin sulfate, piperacillin and tobramycin. The compatibility and duration of stability of drug mixtures will vary depending on concentration and other conditions. No incompatibility has been demonstrated with the antibiotics cephalothin, kanamycin, gentamicin, penicillin or carbenicillin. The following drugs are physically incompatible with DACLIN :
Ampicillin, phenytoin sodium, barbiturates, aminophylline, calcium gluconate, magnesium sulphate, ceftriaxone sodium and ciprofloxacin.
CONTRAINDICATIONS :
This drug is contraindicated in individuals with a history of hypersensitivity to preparations containing Clindamycin or lincomycin. Since Clindamycin does not diffuse adequately into the cerebrospinal fluid, the medicine should not be used in the treatment of meningitis.
WARNINGS :
SERIOUS ANAPHYLACTOID REACTIONS REQUIRE IMMEDIATE EMERGENCY TREATMENT WITH ADRENALINE. OXYGEN AND INTRAVENOUS CORTICOSTEROIDS SHOULD ALSO BE ADMINISTERED AS INDICATED.
The use of Clindamycin can lead to the development of severe colitis. Fatalities have been reported. Therefore, DACLIN should be reserved for serious infections where less toxic antimicrobial agents are inappropriate. It should not be used in patients with non-bacterial infections such as most upper respiratory tract infections. A toxin produced by Clostridium difficile appears to be the primary cause. The severity of the colitis may range from mild to life threatening. It is important to consider this diagnosis in patients who develop diarrhoea or colitis in association with the use of antibiotics, including parenteral Clindamycin. Symptoms may occur up to several weeks after cessation of antibiotic therapy. Cholestyramine and colestipol resins have been shown to bind the toxin in vitro. The colitis is usually characterized by mild watery diarrhoea to severe, persistent diarrhoea, leukocytosis, fever, severe abdominal cramps which may be associated with the passage of blood and mucous and if allowed to progress may produce peritonitis, shock and toxic megacolon. Endoscopic examination may reveal pseudomembranous colitis.
Mild cases of pseudomembranous colitis usually respond to drug discontinuation alone, however in moderate to severe cases appropriate therapy with suitable oral antibacterial agents effective against Clostridium difficile should be considered. Fluids, electrolytes and protein replacement should be provided when indicated. When significant diarrhoea occurs, the drug should be discontinued or, if necessary, continued only with close observation of the patient. Large bowel endoscopy has been recommended. Vancomycin has been found to be effective in the treatment of antibiotic associated pseudomembranous colitis produced by Clostridium difficile. The usual adult dose is 500 mg to 2 g of vancomycin orally per day in three to four divided doses administered for seven to ten days.
If both a resin and vancomycin are to be administered concurrently, it may be advisable to separate the time of administration of each drug. Diarrhoea, colitis, and pseudomembranous colitis have been observed to begin up to several weeks following cessation of therapy with Clindamycin. Systemic corticoids and corticoid retention enemas may help relieve the colitis. Other causes of colitis should also be considered. Antibiotic-associated colitis and diarrhoea (due to C. difficile), occur more frequently and may be more severe in debilitated and/or elderly patients (> 60 years). When Clindamycin is indicated in these patients, they should be carefully monitored for change in bowel frequency. DACLIN should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis. DACLIN should be prescribed with caution in atopic individuals. During prolonged therapy periodic liver and kidney function tests and blood counts should be performed. Patients with very severe renal disease and/or very severe hepatic disease accompanied by severe, metabolic aberrations should be dosed with caution, and serum Clindamycin levels monitored during high-dose therapy. Indicated surgical procedures should be performed in conjunction with antibiotic therapy. The use of DACLIN may result in overgrowth of nonsusceptible organisms - particularly yeasts. Should superinfections occur, appropriate measures should be taken as indicated by the clinical situation. DACLIN should not be injected intravenously undiluted as a bolus, but should be infused over at least 10-60 minutes . Drugs which delay peristalsis (e.g., opiates and diphenoxylate with atropine) may prolong and/or worsen the condition and should not be used. DACLIN should be used with caution in patients with a history of regional enteritis, ulcerative colitis or antibiotic associated colitis. Stool culture for Clostridium difficile and stool assay for C. difficile toxin maybe helpful diagnostically.
PRECAUTIONS :
This product contains benzyl alcohol as preservative. Benzyl alcohol has been reported to be associated with a fatal "Gasping Syndrome" in premature infants. Symptoms include a striking onset of gasping syndrome, hypotension, bradycardia and cardiovascular collapse.
Use in Pregnancy : Pregnancy Category A
Clindamycin crosses the placenta in humans. After multiple doses, amniotic fluid concentrations were approximately 30 % of maternal concentrations. Clindamycin should be used in pregnancy only if clearly needed.
Use in Lactation :
Clindamycin has been reported to appear in breast milk in ranges of 0.7 to 3.8 micrograms/mL, therefore, it is not recommended for nursing mothers.
INTERACTIONS :
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents. Antagonism has been demonstrated between DACLIN and erythromycin in vitro. Because of possible clinical significance these two drugs should not administered concurrently.
SIDE EFFECTS :
The following side effects have been reported with the use of Clindamycin.
Gastrointestinal : Abdominal pain, nausea, vomiting and diarrhoea.
Hypersensitivity Reactions : Maculopapular rash and urticaria have been observed during drug therapy. Generalised mild to moderate morbilliform-like skin rashes are the most frequently reported of all adverse reactions. Rare instances of erythema multiforme, some resembling Stevens-Johnson Syndrome, have been associated with Clindamycin. A few cases of anaphylactoid reactions have been reported. If a hypersensitivity reaction occurs, the drug should be discontinued. The usual agents (adrenaline, corticosteroids, colloid infusion, antihistamines) should be available for emergency treatment of serious reactions.
Liver : Jaundice and abnormalities in liver function tests have been observed during Clindamycin therapy.
Skin and Mucous Membranes : Pruritis, skin rashes, urticaria, vaginitis and rare instances of exfoliative and vesiculobullous dermatitis have been reported.Rare cases of toxic epidermal necrolysis have been reported.
Haemopoietic : Transient neutropenia (leucopenia) and eosinophilia have been reported. Rare cases of agranulocytosis and thrombocytopenia have been reported. No direct cause/effect relationship to concurrent Clindamycin therapy could be made in any of the foregoing.
Cardiovascular : Rare instances of cardiopulmonary arrest and hypotension have been reported following too rapid intravenous administration.
Musculoskeletal : Rare instances of polyarthritis have been reported.
Nervous System : Dysgeusia.
Local Reactions : Local irritation, pain, induration and sterile abscess have been reported after intramuscular injection and thrombophlebitis after intravenous infusion. Reactions can be minimised by giving deep intramuscular injections and avoiding prolonged use of indwelling intravenous catheters.
OVERDOSAGE :
The sign and symptoms of overdosage are quantitatively similar to the side effects.
TREATMENT OF OVERDOSAGE :
In cases of overdosage no specific treatment is indicated.
The serum biological half-life of lincomycin is 2.4 hours. Clindamycin cannot readily be removed from the blood by dialysis or peritoneal dialysis.
If an allergic adverse reaction occurs, therapy should be with the usual emergency treatments, including corticosteroids, adrenaline and antihistamines.
PHARMACEUTICAL PRECAUTIONS :
Parenteral drug products should be inspected visually for particulate matter and discolouration prior to administration, whenever solution and container permit.
STORAGE :
Store below 30°C (86°F).
Do not refrigerate.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
DACLIN is supplied as per below table.
-Table-2.jpg)
Disclaimer : For the use of a Registered Medical Practitioner or a Hospital or a Institution only. Also it is not intended to be used by healthcare professionals or patients for the purpose of prescribing or administering these products. Questions regarding the complete and current content of product labeling / specification / presentation should be directed to SGPharma.

 Cardiovascular
Cardiovascular








