250 mg/10 ml
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
MEXILATE (Mexiletine Injection B.P.) is Class I Antiarrhythmic. Chemically, Mexiletine Hydrochloride is (2RS)-1-(2,6-Dimethylphenoxy)propan-2-amine hydrochloride. The molecular formula is C11H17NO,HCl. and molecular weight is 215.7
STRUCTURAL FORMULA :
Its structural formula is :
-Structure.jpg)
MEXILATE is a sterile, clear, colourless solution filled in amber OPC ampoule of suitable size.
COMPOSITION :
Each ml contains :
Mexiletine Hydrochloride B.P. 25 mg
Sodium Chloride B.P. 9 mg
Water for Injections B.P. q.s.
ACTIONS :
Mexiletine hydrochloride is a local anaesthetic, antiarrhythmic agent, structurally similar to lidocaine, but orally active. In animal studies, mexiletine has been shown to be effective in the suppression of induced ventricular arrhythmias, including those induced by glycoside toxicity and coronary artery ligation. Mexiletine, like lidocaine, inhibits the inward sodium current, thus reducing the rate of rise of the action potential, Phase 0. Mexiletine decreased the effective refractory period (ERP) in Purkinje fibers. The decrease in ERP was of lesser magnitude than the decrease in action potential duration (APD), with a resulting increase in the ERP/APD ratio. Electrophysiology in Man : Mexiletine is a Class 1B antiarrhythmic compound with electrophysiologic properties in man similar to those of lidocaine, but dissimilar from quinidine, procainamide, and disopyramide.
In patients with normal conduction systems, mexiletine has a minimal effect on cardiac impulse generation and propagation. In clinical trials, no development of second-degree or third-degree AV block was observed. Mexiletine did not prolong ventricular depolarization (QRS duration) or repolarization (QT intervals) as measured by electrocardiography. Theoretically, therefore, mexiletine may be useful in the treatment of ventricular arrhythmias associated with a prolonged QT interval. In patients with pre-existing conduction defects, depression of the sinus rate, prolongation of sinus node recovery time, decreased conduction velocity and increased effective refractory period of the intraventricular conduction system have occasionally been observed. The antiarrhythmic effect of mexiletine has been established in controlled comparative trials against placebo, quinidine, procainamide, and disopyramide. Mexiletine hydrochloride, at doses of 200 to 400 mg q8h, produced a significant reduction of ventricular premature beats, paired beats, and episodes of non-sustained ventricular tachycardia compared to placebo and was similar in effectiveness to the active agents. Among all patients entered into the studies, about 30 % in each treatment group had a 70 % or greater reduction in PVC count and about 40 % failed to complete the 3 month studies because of adverse effects. Follow-up of patients from the controlled trials has demonstrated continued effectiveness of mexiletine in long-term use.
Haemodynamics :
Haemodynamic studies in a limited number of patients, with normal or abnormal myocardial function, following oral administration of mexiletine hydrochloride, have shown small, usually not statistically significant, decreases in cardiac output and increases in systemic vascular resistance, but no significant negative inotropic effect. Blood pressure and pulse rate remain essentially unchanged. Mild depression of myocardial function, similar to that produced by lidocaine, has occasionally been observed following intravenous mexiletine hydrochloride therapy in patients with cardiac disease.
PHARMACOKINETICS :
Mexiletine is readily and almost completely absorbed from the gastrointestinal tract, with a bioavailability of about 90 %, although absorption may be delayed in situations where gastric emptying is slowed, such as acute myocardial infarction. Mexiletine is metabolised in the liver to a number of metabolites; metabolism may involve cytochrome P450 isoenzymes CYP1A2, CYP2D6, and CYP3A4, and genetic polymorphism in relation to CYP2D6 has been identified. Mexiletine is excreted in the urine, mainly in the form of its metabolites with about 10 % excreted unchanged; clearance is increased in acid urine. Mexiletine is widely distributed throughout the body and is about 50 to 70 % bound to plasma proteins. Mexiletine crosses the placenta and is distributed into breast milk. It has an elimination half-life of about 10 hours in healthy subjects but this may be prolonged in patients with heart disease, hepatic impairment, or severe renal impairment. Its therapeutic effect has been correlated with plasma concentrations of 0.5 to 2 micrograms/ml, but the margin between therapeutic and toxic concentrations is narrow, and severe toxicity may occur within this range.
INDICATIONS :
MEXILATE is indicated for the treatment of documented ventricular arrhythmias, such as sustained ventricular tachycardia, that, in the judgment of the physician, are life-threatening. Because of the proarrhythmic effects of MEXILATE, its use with lesser arrhythmias is generally not recommended. Treatment of patients with asymptomatic ventricular premature contractions should be avoided. Initiation of MEXILATE treatment, as with other antiarrhythmic agents used to treat life-threatening arrhythmias, should be carried out in the hospital. Antiarrhythmic drugs have not been shown to enhance survival in patients with ventricular arrhythmias.
Administration :
For slow intravenous Injection.
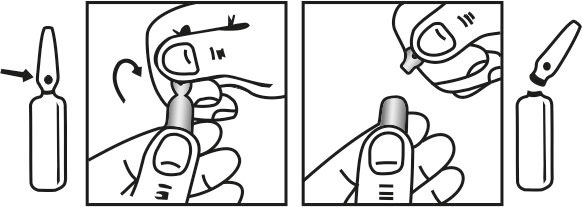
INSTRUCTIONS FOR USE OF AMPOULE :
The ampoule used in this product is equipped with O.P.C (One Point Cut) opening system. No ampoule file is needed to open the ampoule. The neck of the ampoule is prescored at the point of constriction. A coloured dot on the ampoule head helps to orientate the ampoule. Take the ampoule and face the coloured dot. Let the solution at the head of the ampoule to flow down by shaking or a gentle stroke. The ampoule opens easily by placing the thumb on the coloured dot and gently pressing downwards as shown.
Dosage :
Mexiletine hydrochloride may be given by slow intravenous injection in doses of 100 to 250 mg at a rate of 25 mg/minute, followed by an infusion at a rate of 250 mg over 1 hour, 250 mg over the next 2 hours, and then at about 500 micrograms/minute for maintenance, according to response; when appropriate the patient may be transferred to oral therapy with doses of 200 to 250 mg three or four times daily. Alternatively, an initial intravenous dose of 200 mg at a rate of 25 mg/minute, may be followed by an oral dose of 400 mg on completion of the injection, with subsequent oral therapy.
Directions for Use :
For intravenous administration only.
Administration in children :
Mexiletine may be effective for ventricular arrhythmias in children ; a study of 42 children and young adults (age range 5 months to 34 years) found that mexiletine, given orally in a dose of 1.4 to 5 mg/kg every 8 hours, was effective in 30 patients (71 %), with long-term control reported in 18. Treatment was more effective in children with congenital heart disease than in those with cardiomyopathy or no heart disease. Another report found that young children required higher mg/kg doses than adults; a 2-week-old girl and a 20-month-old boy required oral doses of 25 and 15 mg/kg daily, respectively, to produce therapeutic plasma concentrations and control of tachycardia an effective antiarrhythmic drug for treatment of ventricular arrhythmias in congenital heart disease.
Administration in the elderly :
The rate of absorption of mexiletine was slower in a group of 7 elderly subjects compared with 8 young subjects given mexiletine 100 mg by mouth, but the extent of absorption was probably not affected. Elimination of mexiletine was not significantly different between the groups and there was no pharmacokinetic basis for dosage modification of mexiletine in the elderly. An observational study in patients receiving mexiletine found a small decrease in clearance with age, but again this was not considered to warrant dosage adjustment.
Administration in renal impairment :
The pharmacokinetics of mexiletine do not appear to be affected by renal impairment, although one study found that in patients with creatinine clearance below 10 ml/minute the steady-state plasma concentration and half-life were increased, suggesting that dosage should be adjusted according to plasma concentrations in such patients. Haemodialysis and continuous ambulatory peritoneal dialysis do not appear to affect mexiletine clearance.
CONTRAINDICATIONS :
MEXILATE is contraindicated in the presence of cardiogenic shock or pre-existing second- or third-degree AV block (if no pacemaker is present).
WARNINGS AND PRECAUTIONS :
WARNINGS Mortality : In the National Heart, Lung and Blood Institute’s Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multicentered, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days but less than two years previously, an excessive mortality or non-fatal cardiac arrest rate (7.7 %) was seen in patients treated with encainide or flecainide compared with that seen in patients assigned to carefully matched placebo-treated groups (3.0 %). The average duration of treatment with encainide or flecainide in this study was ten months. The applicability of the CAST results to other populations (e.g. those without recent myocardial infarction) is uncertain. Considering the known proarrhythmic properties of mexiletine and the lack of evidence of improved survival for any antiarrhythmic drug in patients without life-threatening arrhythmias, the use of MEXILATE as well as other antiarrhythmic agents should be reversed for patients with life-threatening ventricular arrhythmia.
Acute Liver Injury :
In post-marketing experience abnormal liver function tests have been reported, some in the first few weeks of therapy with MEXILATE Most of these have been observed in the setting of congestive heart failure or ischemia and their relationship to MEXILATE has not been established.
PRECAUTIONS
General :
If a ventricular pacemaker is operative, patients with second or third degree heart block may be treated with MEXILATE if continuously monitored. A limited number of patients (45 of 475 in controlled clinical trials) with pre-existing first degree AV block were treated with MEXILATE ; none of these patients developed second or third degree AV block. Caution should be exercised when it is used in such patients or in patients with pre-existing sinus node dysfunction or intraventricular conduction abnormalities. Like other antiarrhythmics MEXILATE can cause worsening of arrhythmias. This has been uncommon in patients with less serious arrhythmia (frequent premature beats or non-sustained ventricular tachycardia, but is of greater concern in patients with life-threatening arrhythmias such as sustained ventricular tachycardia. In patients with such arrhythmias subjected to programmed electrical stimulation or to exercise provocation, 10-15 % of patients had exacerbation of the arrhythmia, a rate not greater than that of other agents.
MEXILATE should be used with caution in patients with hypotension and severe congestive heart failure because of the potential for aggravating these conditions. Since MEXILATE is metabolized in the liver, and hepatic impairment has been reported to prolong the elimination half-life of MEXILATE patients with liver disease should be followed carefully while receiving MEXILATE The same caution should be observed in patients with hepatic dysfunction secondary to congestive heart failure. Concurrent drug therapy or dietary regimens which may markedly alter urinary pH should be avoided during MEXILATE therapy. The minor fluctuations in urinary pH associated with normal diet do not affect the excretion of MEXILATE
Blood Dyscrasias
Among 10,867 patients treated with mexiletine in the compassionate use program, marked leukopaenia (neutrophils less than 1000/mm3) or agranulocytosis were seen in 0.06 % and milder depressions of leukocytes were seen in 0.08 %, and thrombocytopenia was observed in 0.16 %. Many of these patients were seriously ill and receiving concomitant medications with known haematologic adverse effects. Rechallenge with mexiletine in several cases was negative. Marked leukopaenia or agranulocytosis did not occur in any patient receiving MEXILATE alone ; five of the six cases of agranulocytosis were associated with procainamide (sustained release preparations in four) and one with vinblastine. If significant haematologic changes are observed, the patient should be carefully evaluated, and, if warranted, MEXILATE should be discontinued. Blood counts usually return to normal within one month of discontinuation Convulsions (seizures) did not occur in MEXILATE controlled clinical trials. In the compassionate use program, convulsions were reported in about 2 of 1000 patients. Twenty-eight percent of these patients discontinued therapy. Convulsions were reported in patients with and without a prior history of seizures. Mexiletine should be used with caution in patients with known seizure disorder.
Pregnancy : Category C.
Reproduction studies performed with mexiletine hydrochloride in rats, mice, and rabbits at doses up to four times the maximum human oral dose (24 mg/Kg in a 50 Kg patient) revealed no evidence of teratogenicity or impaired fertility but did show an increase in foetal resorption. There are no adequate and well-controlled studies in pregnant women; this drug should be used in pregnancy only if the potential benefit justifies the potential risk to the foetus.
Nursing mother :
Mexiletine appears in human milk in concentrations similar to those observed in plasma. Therefore, if the use of mexiletine is deemed essential, an alternative method of infant feeding should be considered.
Paediatric use :
Safety and effectiveness in paediatric patients have not been established.
INTERACTIONS AND INCOMPABILITIES :
Mexiletine undergoes extensive metabolism in the liver particularly by the cytochrome P450 isoenzymes CYP1A2 and CYP2D6, and possibly CYP3A4, and interactions may occur with other drugs metabolized by the same enzymes. Plasma concentrations of mexiletine may be reduced by hepatic enzyme inducers such as phenytoin and rifampicin; increased plasma concentrations may occur with enzyme inhibitors. Absorption of mexiletine may be delayed by drugs that slow gastric emptying such as opioid analgesics and atropine. The rate of absorption may be increased by metoclopramide; the extent of absorption is unaffected. Drugs that acidify or alkalinizes the urine enhance or reduce the rate of elimination of mexiletine, respectively. There may be an increased risk of arrhythmias if mexiletine is used with other antiarrhythmics or with arrhythmogenic drugs. Mexiletine has been reported to increase theophylline concentration and to precipitate lidocaine toxicity.
SIDE EFFECTS :
MEXILATE has a narrow therapeutic ratio ; many adverse effects of MEXILATE are dose-related and will respond to dosage reduction but may be severe enough to force mexiletine to be stopped and symptomatic and supportive therapy to be given. Toxicity is common with oral or parenteral loading doses when plasma concentrations are high. The most common adverse effects involve the gastrointestinal tract and CNS. Effects on the gastrointestinal tract include nausea, vomiting, constipation, and diarrhoea; oesophageal ulceration has also been reported. Effects on the nervous system include tremor, confusion, lightheadedness, dizziness, blurred vision and other visual disturbances, sleep disturbances, and speech difficulties. The most frequent cardiovascular effects are hypotension, sinus bradycardia, heart block and AV dissociation, and atrial fibrillation. As with other antiarrhythmics MEXILATE may exacerbate arrhythmias. Other adverse effects that have been reported include skin rashes, abnormal liver function tests, thrombocytopenia, positive antinuclear factor titres, and convulsions. The Stevens-Johnson syndrome has been reported rarely.
OVERDOSAGE :
Clinical findings associated with MEXILATE overdosage have included drowsiness, confusion, nausea, hypotension, sinus bradycardia, paresthesia, seizures, bundle branch block, AV heart block, asystole, ventricular tachyarrhythmia, including ventricular fibrillation, cardiovascular collapse and coma. The lowest known dose in a fatality case was 4.4g with postmortem serum mexiletine level of 34-37 mcg/ml Patients have recovered from ingestion of 4 g to 18 g of mexiletine.
TREATMENT OF OVERDOSAGE :
There is no specific antidote for MEXILATE Management of MEXILATE overdosage includes general supportive measures, close observation and monitoring of vital signs. In addition, the use of pharmacologic interventions (e.g., pressor agents, atropine or anticonvulsants) or transvenous cardiac pacing is suggested, depending on the patient’s clinical condition.
PHARMACEUTICAL PRECAUTIONS :
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
STORAGE :
Store below 25°C (77°F), protected from light.
Do not refrigerate.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
MEXILATE (Mexiletine Injection B.P.) is supplied as
25 mg/ml of Mexiletine Hydrochloride B.P. in 10 ml aqueous solution.
Such 5 Ampoules of 10 ml is packed in a Box.
Disclaimer : For the use of a Registered Medical Practitioner or a Hospital or a Institution only. Also it is not intended to be used by healthcare professionals or patients for the purpose of prescribing or administering these products. Questions regarding the complete and current content of product labeling / specification / presentation should be directed to SGPharma.

 Cardiovascular
Cardiovascular