0.2 mg/ml, 2 mg/ml
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
ISOSOL (Isoprenaline Hydrochloride) is a synthetic sympathomimetic amine that is structurally related to epinephrine but acts almost exclusively on beta receptors. Chemically, Isoprenaline Hydrochloride is 3,4-Dihydroxy-α-[(isopropylamino) methyl]-benzyl alcohol hydrochloride. The molecular formula is C11H17NO3·HCl and molecular weight is 247.72.
STRUCTURAL FORMULA :
Its structural formula is :
-structure.jpg)
ISOSOL is a clear colourless sterile solution filled in amber glass ampoule of suitable size.
COMPOSITION :
ISOSOL
Each ml contains :
Isoprenaline HCl I.P. 0.2 mg
Water for Injections I.P. q.s.
Contains no preservatives.
ISOSOL
Each ml contains :
Isoprenaline HCl I.P. 1 mg
Water for Injections I.P. q.s.
Contains no preservatives.
ISOSOL
Each ml contains :
Isoprenaline HCl I.P. 2 mg
Water for Injections I.P. q.s.
Contains no preservatives.
ACTIONS :
Isoprenaline is a potent non selective beta-adrenergic agonist with low affinity for alpha-adrenergic receptors. Isoprenaline acts primarily on the heart and on smooth muscle of bronchi, skeletal muscle vasculature and the gastrointestinal tract. Isoprenaline increases cardiac output due to its positive inotropic and chronotropic actions and increasing venous return. With usual therapeutic doses, the increase in cardiac output is generally sufficient to maintain or increase systolic blood pressure. Intravenous infusion of Isoprenaline also lowers peripheral vascular resistance. The diastolic pressure, therefore, may be expected to fall in normal individuals. Thus the mean pressure may be reduced. The rate of discharge of cardiac pacemakers is increased with Isoprenaline. Isoprenaline relaxes most smooth muscle, the most pronounced effect being on bronchial and gastrointestinal smooth muscle. It produces marked relaxation in the smaller bronchi and may even dilate the trachea and main bronchi past the resting diameter. In man, Isoprenaline causes less hyperglycaemia than does adrenaline. Isoprenaline and adrenaline are equally effective in stimulating the release of free fatty acids and energy production.
PHARMACOKINETICS :
Isoprenaline is readily absorbed when given parenterally.
The half-life of isoprenaline hydrochloride is brief lasting only a few minutes following intravenous administration and up to 2 hours after subcutaneous administration. Isoprenaline is metabolised by catechol-o-methyl transferase primarily in the liver. The major metabolite after intravenous administration is 3-0-methylisoprenaline, which is reported to have weak β-adrenergic blocking activity, and its conjugates. Isoprenaline is a relatively poor substrate for MAO and is not taken up by sympathetic neurons to the same extent as adrenaline and noradrenaline. The duration of action of isoprenaline may therefore be longer than that of adrenaline, but it is still brief. The metabolites are excreted through the kidneys.
INDICATIONS :
ISOSOL is indicated for :
1. Mild or transient episodes of heart block that do not require electric shock or pacemaker therapy.
2. Serious episodes of heart block and Adams-Stokes attacks (except when caused by ventricular tachycardia or fibrillation).
3. Use in cardiac arrest until electric shock or pacemaker therapy, the treatments of choice, is available.
4.Bronchospasm occurring during anaesthesia.
5.As an adjunct to fluid and electrolyte replacement therapy and the use of other drugs and procedures in the treatment of hypovolaemic and septic shock, low cardiac output (hypop erfusion) states, congestive heart failure and cardiogenic shock.
ISOSOL can be administered by the intravenous, intramuscular, subcutaneous or intracardiac routes.
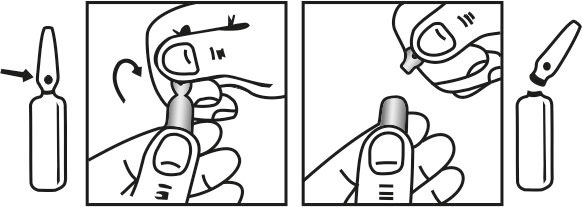
INSTRUCTIONS FOR USE OF AMPOULE :
The ampoule used in this product is equipped with O.P.C (One Point Cut) opening system. No ampoule file is needed to open the ampoule. The neck of the ampoule is prescored at the point of constriction. A coloured dot on the ampoule head helps to orientate the ampoule. Take the ampoule and face the coloured dot. Let the solution at the head of the ampoule to flow down by shaking or a gentle stroke. The ampoule opens easily by placing the thumb on the coloured dot and gently pressing downwards as shown.
Dosage :
ISOSOL should generally be started at the lowest recommended dose and the rate of administration gradually increased if necessary while carefully monitoring the patient. The usual route of administration is by intravenous infusion or bolus intravenous injection. In dire emergencies, the medicine may be administered by intracardiac injection. If time is not of the utmost importance, initial therapy by intramuscular or subcutaneous injection is preferred. Elderly patients may be more sensitive to the effects of sympathomimetics and lower doses may be required.
Adults :
Recommended Dosage for adults with shock and hypoperfusion states
-table-1.jpg)
+ Concentrations up to 10 times greater have been used when limitation of volume is essential. ++ Rates over 30 mcg per minute have been used in advanced stages of shock. The rate of infusion should be adjusted on the basis of heart rate, central venous pressure, systemic blood pressure, and urine flow. If the heart rate exceeds 110 beats per minute, it may be advisable to decrease or temporarily discontinue the infusion.
Recommended dosage for adults with heart block, Adams-Stokes attacks and cardiac arrest
|
Route of Administration |
Preparation of dilution | Initial Dose | Subsequent Administration dose range* |
|---|---|---|---|
|
Bolus Intravenous Injection |
Dilute 0.2 mg to 2 ml with sodium chloride injection |
0.02 mg to 0.06 mg |
0.01 mg to 0.02 mg |
|
Intravenous Infusion |
Dilute 2 mg in 500 ml of 5% Dextrose Injection I.P. |
5 mcg/min |
|
|
Intramascular |
Use Solution 0.2 mg Undiluted |
0.2 mg |
0.02 mg to 1 mg |
|
Subcuataneous |
Use Solution 0.2 mg Undiluted |
0.2 mg |
0.15 mg to 0.2 mg |
|
Intracardiac |
Use Solution 0.2 mg Undiluted |
0.2 mg |
|
* Subsequent dosage and method of administration depend on the ventricular rate and the rapidity with which the cardiac pacemaker can take over when the medicine is gradually withdrawn.
Recommended dosage for adults with bronchospasm occurring during anaesthesia
-table-3.jpg)
Children :
There are no well-controlled studies in children to establish appropriate dosing; however, the American Heart Association recommends an initial infusion rate of 0.1 mcg/kg/min, with the usual range being 0.1 mcg/kg/min to 1.0 mcg/kg/min. Adequacy and safety of intravenous isoprenaline in children are not established. Based on published literature, the initial dose of intravenous isoprenaline used in children is not established. Based on published literature, the initial dose of intravenous isoprenaline used in children (age 7 to 19 years of age) ranges between 0.05 to 0.17 mcg/kg/min, which is increased gradually by 0.1 to 0.2 mcg/kg/min at intervals of 15 to 20 minutes, titrated to clinical response; a maximum dose ranging between 1.3 to 2.7 mcg/kg/min has been used. In children generally, post-operative cardiac patients with bradycardia require lower doses (0.029 ± 0.002 mcg/kg/min) of intravenous isoprenaline than asthma patients (0.5 ± 0.21 mcg/kg/min).
CONTRAINDICATIONS :
Use of ISOSOL is contraindicated in patients with tachyarrhythmias; tachycardia or heart block caused by digitalis intoxication; ventricular arrhythmias which require inotropic therapy; and angina pectoris.
WARNINGS :
ISOSOL, by increasing myocardial oxygen requirements while decreasing effective coronary perfusion, may have a deleterious effect on the injured or failing heart. Most experts discourage its use as the initial agent in treating cardiogenic shock following myocardial infarction. However, when a low arterial pressure has been elevated by other means, Isoprenaline Injection may produce beneficial haemodynamic and metabolic effects. In a few patients, presumably with organic disease of the AV node and its branches, Isoprenaline Injection has paradoxically been reported to worsen heart block or to precipitate Adams-Stokes attacks during normal sinus rhythm or transient heart block.
PRECAUTIONS :
ISOSOL should generally be started at the lowest recommended dose. This may be gradually increased if necessary while carefully monitoring the patient. ISOSOL contains sodium metabisulphite, a sulphite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulphite sensitivity in the general population is unknown and probably low. Sulphite sensitivity is seen more frequently in asthmatic than non-asthmatic people. Particular caution is necessary in administering Isoprenaline injection to the elderly and patients with coronary insufficient, ischaemic heart disease, hypertension, aneurysms, diabetes or hyperthyroidism and in patients sensitive to sympathomimetic amines. There are case reports of occasional fatal cardiac dysrhythmia and myocardial necrosis at autopsy as a result of intravenous isoprenaline. ECG changes and serum CPK-MB level elevation consistent with transient myocardial ischaemia and abnormal echocardiographic findings suggestive of myocardial dysfunction have been documented with the use of intravenous isoprenaline infusion for the treatment of severe asthma exacerbations in children. Care should be taken to ensure that oxygen is always administered during isoprenaline infusions in patients with asthma. Heart rate, blood pressure, arrhythmias and evidence of myocardial ischaemia by ECG should be monitored. Arterial blood gases should also be monitored carefully and PaO2 maintained above 60 torr. Where ECG suggests myocardial ischaemia, cardiac enzymes including cardiac-specific CPK-MB isoenzyme levels should be determined. Adequate filling of the intravascular compartment by suitable volume expanders is of primary importance in most cases of shock and should precede the administration of vasoactive drugs. In patients with normal cardiac function, determination of central venous pressure is a reliable guide during volume replacement. If evidence of hypoperfusion persists after adequate volume replacement, ISOSOL may be given.
Determinations of cardiac output and circulation time may also be helpful. Doses of ISOSOL sufficient to increase the heart rate to a more than 130 beats per minute may induce ventricular arrhythmia. If the cardiac rate increases sharply, patients with angina pectoris may experience anginal pain until the cardiac rate decreases. If ventricular hyperexcitability (extrasystoles, polymorphic extrasystoles or sustained ventricular tachycardia) should occur, the dosage should be reduced and the electrocardiogram monitored. Appropriate measures should be taken to ensure adequate ventilation. Careful attention should be paid to acid-base balance and to the correction of electrolyte disturbances.
Use in Pregnancy : Category C
Animal reproduction studies have not been conducted with isoprenaline hydrochloride. It is also not known whether isoprenaline hydrochloride can cause foetal harm when administered to a pregnant woman or can affect reproduction capacity. isoprenaline hydrochloride should be given to a pregnant woman only if clearly needed.
Nursing mothers :
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ISOSOL is administered to a nursing woman.
Paediatric Use :
Safety and efficacy of isoprenaline in paediatric patients have not been established. Intravenous infusions of isoprenaline in refractory asthmatic children at rates of 0.05 - 2.7 µg/kg/min have caused clinical deterioration, myocardial necrosis, congestive heart failure and death. The risks of cardiac toxicity appear to be increased by some factors [acidosis, hypoxemia, coadministration of corticosteroids, coadministration of methylxanthines (theophylline, theobromine) or aminophylline] that are especially likely to be present in these patients. If IV isoprenaline is used in children with refractory asthma, patient monitoring must include continuous assessment of vital signs, frequent electrocardiography, and daily measurements of cardiac enzymes, including CPK-MB.
INTERACTIONS :
Adrenaline :
ISOSOL and adrenaline should not be administered simultaneously because both medicines are direct cardiac stimulants and their combined effects may induce serious arrhythmias. The medicines may, however, be administered alternately provided a proper interval has elapsed between doses.
Anaesthetics :
ISOSOL should be used with caution, if at all, when potent inhalational anaesthetics such as halothane and cyclopropane are employed because of potential to sensitise the myocardium to effects of sympathomimetic amines.
Antidepressants, tricyclic or Maprotiline :
Concurrent use may potentiate cardiovascular effects of isoprenaline and phenylephrine, possibly resulting in arrhythmias, tachycardia or severe hypertension or hyperpyrexia.
Beta-adrenergic blocking agents :
Concurrent use with isoprenaline may result in mutual inhibition of therapeutic effects; beta-blockade may antagonise beta-2-adrenergic bronchodilating effects of isoprenaline; use of a cardioselective beta-2-adrenergic blocker, such as acebutolol, atenolol, or metoprolol, at low doses may reduce antagonism of the bronchodilating effect.
CNS Stimulants :
Concurrent use with isoprenaline may result in additive CNS stimulation to excessive levels, which may cause unwanted effects such as nervousness, irritability, insomnia, or possibly convulsions or cardiac arrhythmias; close observation is recommended.
Digitalis Glycosides :
Concurrent use with isoprenaline and phenylephrine may increase the risk of cardiac arrhythmias; caution and electrocardiographic monitoring are very important if concurrent use is necessary.
Thyroid hormones :
Concurrent use may increase the effects of either these medications or isoprenaline and phenylephrine; thyroid hormones enhance risk of coronary insufficiency when sympathomimetic agents are administered to patients with coronary artery disease; dosage adjustment is recommended, although problem is reduced in euthyroid patients.
MAOI’s, Chlorpromazine :
Isoprenaline should not be used with chlorpromazine or monoamine oxidase inhabitors since the effects of isoprenaline may be magnified.
Xanthines/Corticosteroids :
Caution should be maintained when using continuous intravenous isoprenaline infusions in conjunction with intravenous methyl xanthines (aminophylline, theophylline) and intravenous corticosteroids. The use of isoprenaline with aminophylline and corticosteroids may be additive in cardiotoxic properties and can lead to myocardial necrosis and death. Severe cardiac symptoms of sympathetic overactivation i.e. hypertension, tachycardia, arrhythmias, seizures, myocardial ischaemia and fatal myocardial necrosis, have been reported.
SIDE EFFECTS :
Serious reactions to Isoprenaline Injection are Infrequent. The following reactions, however, have been reported :
CNS :
Nervousness, headache, dizziness.
Cardiovascular :
Tachycardia, palpitations, angina, Adams-Stokes attacks, pulmonary oedema, hypertension, hypotension, ventricular arrhythmias, tachyarrhythmias. In a few patients, presumably with organic disease of the AV node and its branches, Isoprenaline Injection has been reported to precipitate Adams-Stokes seizures during normal sinus rhythm or transient heart block.
OVERDOSAGE :
The acute toxicity of Isoprenaline Injection in animals is much less than that of epinephrine. Excessive doses in animals or man can cause a striking drop in blood pressure and repeated large doses in animals may result in cardiac enlargement and focal myocarditis. In case of accidental overdosage as evidenced mainly by tachycardia or other arrhythmias, palpitations, angina, hypotension, or hypertension, reduce rate of administration or discontinue Isoprenaline Injection until patient’s condition stabilizes. Blood pressure, pulse, respiration and ECG should be monitored.
PHARMACEUTICAL PRECAUTIONS :
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
STORAGE :
Store below 30°C (86°F), protected from light.
Do not refrigerate.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
ISOSOL is supplied as below table :
| Strength | Pack SIze | Packing |
| 0.2mg/ml | 1 ml Ampoule | 3 Ampoule per Box |
| 1 mg/ml | 2 ml Ampoule | 3 Ampoule per Box |
| 2 mg/ml | 1 ml Ampoule | 3 Ampoule per Box |
Disclaimer : For the use of a Registered Medical Practitioner or a Hospital or a Institution only. Also it is not intended to be used by healthcare professionals or patients for the purpose of prescribing or administering these products. Questions regarding the complete and current content of product labeling / specification / presentation should be directed to SGPharma.

 Cardiovascular
Cardiovascular