
100 mg
For the use of a Registered Medical Practitioner or a Hospital or a Institution only.
COLISTIMETHATE FOR INJECTION USP (Colistimethate Sodium) is a cyclic polypeptide antibiotic. Chemically, Colistimethate Sodium is pentasodium [[4-[[3-hydroxy-1-[[1-[[3-(1-hydroxyethyl)-12,15-bis(2-methylpropyl)-2,5,8,11,14,17, 20-heptaoxo-6,9,18-tris[2-(sulfonatomethylamino)ethyl]-1,4,7,10,13,16,19-heptazacylotricos-21-yl]amino]-1-oxo-4-(sulfonatomethylamino)butan-2-yl]amino]-1-oxobutan-2-yl]amino]-3-(6-methyloctanoylamino)-4-oxobutyl]amino]methanesulfonate.The molecular formula is C58H105N16Na5O28S5 and molecular weight of 1749.82.
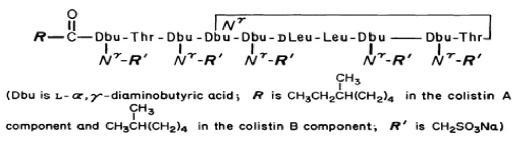
STRUCTURAL FORMULA :
Its structural formula is :
COLISTIMETHATE FOR INJECTION USP is a sterile white to off white powder filled in a amber tubular vial of suitable size.
COMPOSITION :
Each vial contains :
Sterile Colistimethate Sodium USP
equivalent to Colistin 100 mg
ACTIONS :
Colistimethate (also known as colistin) is a cyclic polypeptide antibiotic derived from Bacillus polymyxa var. colistinus and belongs to the polymyxin group. The polymyxin antibiotics are cationic agents that work by damaging the cell membrane. The resulting physiological affects are lethal to the bacterium. Polymyxins are selective for gram-negative bacteria that have a hydrophobic outer membrane.
Resistance :
Resistant bacteria are characterised by modification of the phosphate groups of lipopolysaccharides due to substitution with ethanolamine or aminoarabinose. Naturally resistant Gram-negative bacteria, such as Proteus rnirabilis and Burkholderia cepacia, show complete substitution of their lipid phosphate by ethanolamine or aminoarabinose. Cross-resistance between Colistimethate and polymyxin B would be expected. Since the mechanism of action of the polymyxins is different from that of other antibiotics, resistance to colistimethate and polymyxin by the above mechanism alone would not be expected to result in resistance to other drug classes.
Breakpoints :
The BSAC-recommended general MIC breakpoint to identify bacteria susceptible to Colistimethate is < 4 mg/l. Bacteria for which the MIC of Colistimethate is > 8 mg/I should be considered resistant.
Susceptibility :
The prevalence of resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalence of resistance is such that the utility of the agent in at least some types of infections is questionable.
Commonly susceptible species :
Acinetobacter species*
Citrobacter species
Escherichia coli
Haemophilus influenzae
Pseudomonas aeruginosa
Species for which acquired resistance may be a problem :
Enterobacter species
Klebsiella species
Inherently resistant organisms :
Brucella species
Burkholderia cepacia and related species.
Neisseria species
Proteus species
Providencia species
Serratia species
Anaerobes :
All Gram-positive organisms
*Note that the in-vitro demonstration of susceptibility may not reliably predict clinical efficacy for Acinetobacter species.
PHARMACOKINETICS :
Colistimethate sodium are poorly absorbed from the gastrointestinal tract of adults and children; however, limited and unpredictable gastrointestinal absorption occurs in infants under 6 months of age. The drugs are not absorbed through mucous membranes, or intact or denuded skin. Peak plasma concentrations usually occur 2 to 3 hours after an intramuscular injection of colistimethate sodium. Plasma protein binding of colistin is reported to be more than 50 % but that of colistimethate sodium is low. Colistin is reversibly bound to body tissues, but binding does not occur with colistimethate. Some colistimethate sodium may be hydrolysed to colistin in vivo. The serum half-life of colistimethate sodium is 2 to 3 hours but is prolonged in renal impairment; values of 10 to 20 hours have been reported in patients with a creatinine clearance of less than 20 ml/minute. Half-life may initially be prolonged in neonates but has been reported to fall to 2 to 3 hours after 3 or 4 days. Colistimethate is mainly excreted by glomerular filtration as changed and unchanged drug and up to 80 % of a parenteral dose may be recovered in the urine within 24 hours. Excretion is more rapid in children than in adults; it is reduced in patients with renal impairment. Colistin crosses the placenta but diffusion into the CSF is negligible. It is distributed into breast milk.
INDICATIONS :
COLISTIMETHATE FOR INJECTION USP is indicated for the treatment of acute or chronic infections due to sensitive strains of certain gram-negative bacilli; particularly when the infection is caused by sensitive strains of Pseudomonas aeruginosa, and the gram-negative organisms; Aerobacter aerogenes, Escherichia coli, Klebsiella pneumoniae. COLISTIMETHATE FOR INJECTION USP may be used to initiate therapy in serious infections that are suspected to be due to gram-negative organisms and in the treatment of infections due to susceptible gram-negative pathogenic bacilli. To reduce the development of drug-resistant bacteria and maintain the effectiveness of COLISTIMETHATE FOR INJECTION USP and other antibacterial drugs, COLISTIMETHATE FOR INJECTION USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Administration :
COLISTIMETHATE FOR INJECTION USP is given by intramuscular injection or slow intravenous injection or infusion.
Method of Administration :
Important :
COLISTIMETHATE FOR INJECTION USP is supplied in vials containing colistimethate sodium equivalent to 100 mg colistin base activity per vial.
Reconstitution for Intravenous or Intramuscular Administration :
The 100 mg vial should be reconstituted with 2 ml Sterile Water for Injection USP. The reconstituted solution provides colistimethate sodium at a concentration equivalent to 50 mg/ml colistin base activity. During reconstitution swirl gently to avoid frothing.
Dosage :
Adults and paediatric patients – Intravenous or Intramuscular Administration :
The dose of COLISTIMETHATE FOR INJECTION USP should be 2.5 to 5 mg/kg per day of colistin base in 2 to 4 divided doses for patients with normal renal function, depending on the severity of the infection. In obese individuals, dosage should be based on ideal body weight.
INTRAVENOUS ADMINISTRATION :
1. Direct Intermittent Administration - Slowly inject one-half of the total daily dose over a period of 3 to 5 minutes every 12 hours.
2. Continuous Infusion - Slowly inject one-half of the total daily dose over 3 to 5 minutes. Add the remaining half of the total daily dose of COLISTIMETHATE FOR INJECTION USP to one of the following :
0.9 % NaCl
5 % dextrose in 0.9 % NaCl
5 % dextrose in water
5 % dextrose in 0.45 % NaCl
5 % dextrose in 0.225 % NaCl
Lactated Ringer’s solution
10 % invert sugar solution
There are not sufficient data to recommend usage of COLISTIMETHATE FOR INJECTION USP with other drugs or other than the above listed infusion solutions. Administer the second half of the total daily dose by slow intravenous infusion, starting 1 to 2 hours after the initial dose, over the next 22 to 23 hours. In the presence of impaired renal function, reduce the infusion rate depending on the degree of renal impairment. The choice of intravenous solution and the volume to be employed are dictated by the requirements of fluid and electrolyte management. Any final intravenous infusion solution containing colistimethate sodium should be freshly prepared and used for no longer than 24 hours.
INTRAMUSCULAR ADMINISTRATION :
For Intramuscular Injection, administer by deep intramuscular injection into a large muscle mass (such as the gluteal muscles or lateral part of the thigh). Store reconstituted solution for intramuscular injection in a refrigerator 2° to 8°C (36° to 46°F) or between 20° to 25°
(68° to 77°F) and use within 7 days.
CONTRAINDICATIONS :
COLISTIMETHATE FOR INJECTION USP is contraindicated in patients with hypersensitivity to Colistimethate sodium (also known as colistin) or to polymyxin B. COLISTIMETHATE FOR INJECTION USP is also contraindicated in patients with Myasthenia gravis.
Maximum daily dose should not exceed 5 mg/kg/day (2.3 mg/lb) with normal renal function. Transient neurological disturbances may occur. These include circumoral paraesthesia or numbness, tingling or formication of the extremities, generalized pruritus, vertigo, dizziness, and slurring of speech. For these reasons, patients should be warned not to drive vehicles or use hazardous machinery while on therapy. Reduction of dosage may alleviate symptoms. Therapy need not be discontinued, but such patients should be observed with particular care. Nephrotoxicity can occur and is probably a dose-dependent effect of colistimethate sodium. These manifestations of nephrotoxicity are reversible following discontinuation of the antibiotic.
Overdosage can result in renal insufficiency, muscle weakness, apnoea and Drug Interactions subsection for use concomitantly with other antibiotics and curariform drugs. Respiratory arrest has been reported following intramuscular administration of colistimethate sodium. Impaired renal function increases the possibility of apnoea and neuromuscular blockade following administration of colistimethate sodium. Therefore, it is important to follow recommended dosing guidelines. Clostridium difficile associated diarrhoea, (CDAD) has been reported with use of nearly all antibacterial agents, including COLISTIMETHATE FOR INJECTION USP, and may range in severity from mild diarrhoea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile. C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhoea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
PRECAUTIONS :
General :
Since COLISTIMETHATE FOR INJECTION USP is eliminated mainly by renal excretion, it should be used with caution when the possibility of impaired renal function exists. The decline in renal function with advanced age should be considered. When actual renal impairment is present, COLISTIMETHATE FOR INJECTION USP may be used, but the greatest caution should be exercised and the dosage should be reduced in proportion to the extent of the impairment. Administration of amounts of COLISTIMETHATE FOR INJECTION USP in excess of renal excretory capacity will lead to high serum levels and can result in further impairment of renal function, initiating a cycle which, if not recognized, can lead to acute renal insufficiency, renal shutdown, and further concentration of the antibiotic to toxic levels in the body. At this point, interference of nerve transmission at neuromuscular junctions may occur and result in muscle weakness and apnoea. Signs indicating the development of impaired renal function include : diminishing urine output, rising BUN and serum creatinine and decreased creatinine clearance. Therapy with COLISTIMETHATE FOR INJECTION USP should be discontinued immediately if signs of impaired renal function occur. However, if it is necessary to reinstate the drug, dosing should be adjusted accordingly after drug plasma levels have fallen. Prescribing COLISTIMETHATE FOR INJECTION USP in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Pregnancy : Category C
There are no adequate data from the use of Colistimethate sodium in pregnant women. Animal studies in rats and mice do not indicate teratogenic properties. However, single dose studies in human pregnancy show that Colistimethate crosses the placental barrier and there may be a risk of foetal toxicity if repeated doses are given to pregnant patients. Colistimethate should be used in pregnancy only if the benefit to the mother outweighs the potential risk to the foetus.
Nursing mothers :
Colistimethate is secreted in breast milk, and should be administered to breastfeeding women only when clearly needed.
Paediatric Use :
In clinical studies, colistimethate sodium was administered to the paediatric population (neonates, infants, children and adolescents). Although adverse reactions appear to be similar in the adult and paediatric populations, subjective symptoms of toxicity may not be reported by paediatric patients. Close clinical monitoring of paediatric patients is recommended.
INTERACTIONS :
Neuromuscular blocking drugs and ether should be used with extreme caution in patients receiving colistimethate sodium. Concomitant use of colistimethate sodium with other medicinal products of neurotoxic and/or nephrotoxic potential should be avoided. These include the aminoglycoside antibiotics such as gentamicin, amikacin, netilmicin and tobramycin. There may be an increased risk of nephrotoxicity if given concomitantly with cephalosporin antibiotics.
INCOMPATIBILITIES :
In the absence of compatibility studies, reconstituted Colistimethate sodium must not be mixed with other medicinal products.
SIDE EFFECTS :
The following adverse reactions have been reported :
Gastrointestinal : gastrointestinal upset.
Nervous System : tingling of extremities and tongue, slurred speech, dizziness, vertigo and paraesthesia.
Integumentary : generalized itching, urticaria and rash.
Body as a Whole : fever.
Laboratory Deviations : increased blood urea nitrogen (BUN), elevated creatinine and decreased creatinine clearance.
Respiratory System : respiratory distress and apnoea.
Renal System : nephrotoxicity and decreased urine output. Hypersensitivity reactions including skin rash have been reported. If these occur treatment should be withdrawn. Local irritation at the site of injection may occur.
EFFECTS ON ABILITY TO DRIVE AND USE MACHINE :
During parenteral treatment with Colistimethate sodium neurotoxicity may occur with the possibility of dizziness, confusion or visual disturbance. Patients should be warned not to drive or operate machinery if these effects occur.
INFORMATION FOR PATIENTS :
Patients should be counseled that antibacterial drugs including COLISTIMETHATE FOR INJECTION USP should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When COLISTIMETHATE FOR INJECTION USP is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may
(1) Decrease the effectiveness of the immediate treatment and
(2) Increase the likelihood that bacteria will develop resistance and will not be treatable by COLISTIMETHATE FOR INJECTION USP or other antibacterial drugs in the future.
Diarrhoea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
OVERDOSAGE :
Overdosage with colistimethate sodium can cause neuromuscular blockade characterized by paraesthesia, lethargy, confusion, dizziness, ataxia, nystagmus, disorders of speech and apnoea. Respiratory muscle paralysis may lead to apnoea, respiratory arrest and death. Overdosage with the drug can also cause acute renal failure, manifested as decreased urine output and increases in serum concentrations of BUN and creatinine.
TREATMENT OF OVERDOSAGE :
As in any case of overdose, colistimethate sodium therapy should be discontinued and general supportive measures should be utilized. It is unknown whether colistimethate sodium can be removed by haemodialysis or peritoneal dialysis in overdose cases.
PHARMACEUTICAL PRECAUTIONS :
On reconstitution, parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
STORAGE :
Store below 25°C (77°F), protected from moisture and light.
Do not refrigerate.
Reconstituted Colistimethate sodium solution may be kept for up to 8 hours when not stored above 25°C or for up to 24 hours stored in a refrigerator. From a microbiological point of view, the reconstituted product should be used immediately. If not used immediately, in-house storage times and conditions prior to use are the responsibility of the user and should not be longer than 24 hours in the refrigerator (2 to 8°C) or 8 hours when stored at temperatures not exceeding 25°C.
SHELF LIFE :
24 months from the date of manufacture.
PRESENTATION :
COLISTIMETHATE FOR INJECTION USP is supplied as 100 mg of Sterile Colistimethate Sodium USP equivalent to colistin in 10 ml vial.
Single Vial per Box.
Disclaimer : For the use of a Registered Medical Practitioner or a Hospital or a Institution only. Also it is not intended to be used by healthcare professionals or patients for the purpose of prescribing or administering these products. Questions regarding the complete and current content of product labeling / specification / presentation should be directed to SGPharma.

 Cardiovascular
Cardiovascular





